
We often think of our skeletons as solid, unchanging scaffolding. In reality, bone is living tissue, constantly being broken down and rebuilt. But as we age, that delicate balance can shift. For millions, this leads to osteoporosis—a condition where bones become porous, brittle, and alarmingly susceptible to breaks.
While hip fractures often get the most headlines, the spine is frequently the first place osteoporosis makes its presence known. These are often called “silent” vertebral fractures because they can occur without a fall and sometimes without immediate, sharp pain.
In this guide, we’ll explore why the spine is so vulnerable, how to spot the hidden signs of bone loss, and the proactive steps you can take to keep your back strong for a lifetime.
Understanding the "Silent" Threat
A vertebral compression fracture (VCF) occurs when the bony block (vertebra) in the spine collapses. Unlike a broken arm that happens during a traumatic accident, an osteoporotic spine fracture can be triggered by something as mundane as:
Reaching for a heavy grocery bag.
A forceful sneeze or cough.
Slightly losing your balance and landing hard in a chair.
The reason they are “silent” is that about two-thirds of these fractures go undiagnosed. Many people dismiss the resulting back pain as “just getting older” or a simple muscle strain. However, left untreated, these small collapses can lead to a permanent change in posture, chronic pain, and a significantly higher risk of future fractures.
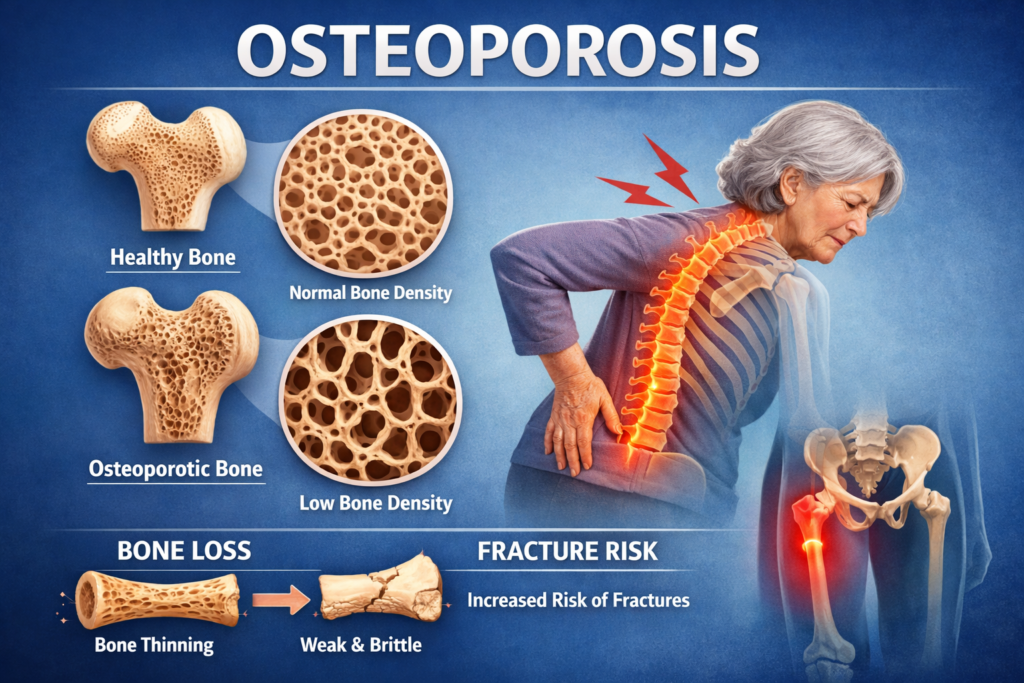
The Anatomy of Bone Loss
To prevent fractures, we have to understand the biology of the bone. Our bodies use a process called remodeling.
Osteoclasts break down old bone.
Osteoblasts build new bone.
By our 30s, we usually reach “peak bone mass.” After that, the breakdown starts to outpace the buildup. In women, the drop in estrogen during menopause accelerates this loss. In men, the decline is more gradual but equally certain. When the internal architecture of the bone—the trabecular bone—thins out, the vertebrae become like hollow eggshells.
5 Signs Your Spine Might Be Changing
1. Loss of Height
If you’ve noticed you are an inch or two shorter than you were in your youth, it’s rarely just “shrinking.” It is often the result of multiple vertebrae compressing.
2. The “Dowager’s Hump” (Kyphosis)
When the front of the vertebrae collapses but the back stays intact, the spine tips forward. This creates a curved upper back, medically known as kyphosis.
3. Sudden Back Pain
While some fractures are painless, others cause a sharp, deep ache that worsens when standing or walking and feels better when lying down.
4. Limited Spinal Mobility
If you find it increasingly difficult to twist your torso or bend over, it may be due to structural changes in the vertebral column.
5. Stomach Issues or Shortness of Breath
In advanced cases, as the spine compresses, there is less room for internal organs. This can lead to digestive issues or reduced lung capacity.
Medical Intervention: Testing and Treatment
If you are over 65 (women) or 70 (men), or younger with risk factors, you should request a DEXA Scan. This is a painless, low-radiation X-ray that measures your Bone Mineral Density (BMD).
If your “T-score” indicates osteoporosis, your doctor may suggest medications:
Bisphosphonates: These slow down the cells that break down bone.
Anabolic Agents: These actually help build new bone (often reserved for high-risk cases).
Hormone Therapy: Can be effective for postmenopausal women.
